Abstract
Background:
Vitamin B1 (Thiamine) deficiency might result in Wernicke's encephalopathy (WE); the latter was reported in clinical studies with the JAK2 inhibitor fedratinib resulting in disruption of clinical development, despite efficacy in patients with myelofibrosis (MF) (JAMA Oncol, 2015, 5). Our objectives were i) to determine the incidence of thiamine deficiency in patients with myeloproliferative neoplasms (MPN), ii) assess clinical correlations of thiamine level and iii) determine the impact of JAK2 inhibitor therapy on thiamine level in MPN.
Methods:
After Institutional review board approval, patients referred with a suspected diagnosis of MPN were enrolled. All clinical and laboratory variables including treatment details were collected at the time of referral. Liquid chromatography-tandem mass spectrometry (LC-MS/MS) analysis of thiamine diphosphate in whole blood was performed at the time of referral. Reference range for thiamine level in whole blood was 70-180 nmol/L. The JMP® Pro 13.0.0 software from SAS Institute, Cary, NC, USA, was used for all statistical analysis.
Results:
A total of 115 patients were prospectively enrolled and included 28 patients without MPN and 87 with MPN. 87 MPN patients (median age, 65 years, 52% males) included 32 with primary myelofibrosis (PMF), 17 with polycythemia vera (PV), 17 with essential thrombocythemia (ET), 11 with post PV MF, 8 with post ET MF, and 2 with MPN-U. The MPN and non-MPN patients were similar in their gender distribution, pattern of alcohol use, malnutrition and multivitamin use (p=0.24, 0.12, 0.54 and 0.78 respectively), although the former were older (p=0.09).
Median thiamine level of the study patients was 167 nmol/L (range; 60-442 nmol/L) with only two (1.7%) female patients displaying level below the normal reference range. One belonged to the non-MPN group (thiamine level 68 nmol/l); a 26 year old female with erythroid leukemia in the absence of alcohol use or malnutrition; the second patient (thiamine level 60 nmol/l) was a 38 year old female with ET, CALR type 2 mutated on hydroxyurea, without a history of alcohol use or malnutrition. Overall, both MPN and non-MPN patients displayed similar thiamine level (p=0.89).
Clinical correlations of thiamine level in MPN
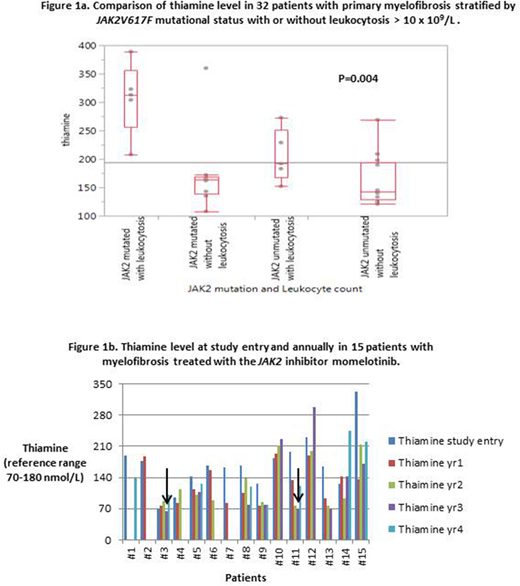
Median thiamine level was similar amongst post ET MF, ET, PMF, PV, and post PV PMF patients (127, 162, 166, 190 and 209 nmol/L respectively, p=0.13). No significant effect on thiamine level was apparent for age, gender, hemoglobin, platelet count, dynamic international prognostic scoring system (DIPSS) score, unfavorable cytogenetics, palpable splenomegaly, or constitutional symptoms. Interestingly, thiamine level was significantly higher in JAK2 mutated cases (median 177 nmol/L vs 145 nmol/L in unmutated cases, p=0.03). Furthermore, when analysis was restricted to PMF patients, thiamine level positively correlated with JAK2V617F mutant allele burden (p=0.01) and leukocyte count > 10 x 109/L (p=0.03). JAK2 mutated PMF patients with leukocyte count > 10 x 109/L depicted significantly higher thiamine levels (median 313 nmol/L) compared to JAK2 mutated patients without leukocytosis (median 164 nmol/L) and JAK2 unmutated patients with or without leukocytosis (median 192 nmol/L and 143 nmol/L respectively)(p=0.004, Figure 1a).
Impact of treatment on thiamine level
Treatment with hydroxyurea was documented in 35 patients with no significant impact on thiamine level (p=0.28). 27 patients were on JAK inhibitors (median duration at referral; 41 months); 12 patients on ruxolitinib and 15 MF patients on momelotinib as part of a clinical trial. Thiamine level was similar amongst JAK inhibitor treated vs untreated patients (median 166 vs 169.5 nmol/L respectively, p=0.72). Annual thiamine measurements were performed on 15 patients treated with momelotinib (median duration 52 months, range 18-60 months). Despite fluctuations in thiamine levels, only two patients were noted to have thiamine level below normal (65 and 69 nmol/L at year 3), which subsequently improved to 101 and 121 nmol/L by year 4, while still on treatment (Figure 1b).
Conclusions:
The current study confirms the rarity of subnormal thiamine levels in MPN and the limited impact of treatment on thiamine levels, including with JAK2 inhibitors. Our novel observation regarding the correlation of thiamine level with JAK2V617F mutant allele burden and leukocyte count requires further exploration.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal